May 22, 2013 New Approaching 1 Year
As my 1 year anniversary approaches, I’m doing great! I’m more active than ever and amazingly have not had any real set backs (knock on wood).
I’ve been going to pilates and a ballet bar style cardio class regularly, and the occasional yoga class. My husband and I just bought bikes and are starting to do a lot more walking and biking now that we live in a more central location. I’ve also started back to the pool for the first time this season now that its hot enough, and the first time I jumped right into the deep end. No more therapy pool for me! I’ve even gotten a little adventurous with some rollerskating and snow tubing! I definitely still feel my muscles waking up when I’m really active or push myself more than usual, but mostly I just get a little stiff when I’ve been sitting at my desk all day with no exercise.
A few weeks ago I finally got my first post op massage. I was nervous about going because the tissue around my screws is still very tender and I was worried about finding a massage therapist who could understand and use the right amount of pressure in the right areas. But she understood perfectly and it was great.
For Memorial Day weekend we have a little getaway in the sun planned with some friends — 4 days of lounging by the pool! Up until now I have been careful to keep my scar out of the sun, so this will be the first time baring it all in daylight! I already have a couple bottles of SPF 100 ready to go.I burn very easily so I want to be really careful with my scar even a year out.
Next month is my 1 year check up appointment. It’s been 9 months since my last one so I’ve definitely made lots of progress since then and am hoping for a clean bill of health. I also have a list of questions prepared:
- I have still been avoiding all NSAIDs. Are they safe to take again?
- My dentist has me taking antibiotics before each cleaning. Is this necessary?
- We are getting closer to being ready for kids. Any reason I shouldn’t get pregnant at this point? Any concerns I should look out for if and when I do?
- Are there any activities I should never do, like rollercoasters for example?
- My stomach sticks out dramatically more on my right side, not just while relaxed, but I can see my right abs engaged more while doing crunches. Is there anything I can do to even it out?
- The tissue around my screws is still sensitive. It’s getting better, but I’m still nervous about getting bumped, etc. Will this continue to improve or I’ll just get used to it?
I will fill you in on the answers or any other news after my appointment.
- 11 comments
- Posted under Uncategorized
September 29, 2012 Almost 4 Months Post Op and feeling good!
Things have continued to improve slowly over the last couple months. Returning to work was tough at first. I was taking a lot of breaks, even lying down for 20 minutes in the afternoon. It was hard to focus for very long, and things like client deadlines seemed so trivial. But being forced to sit upright most of the day really gave me the push I needed to get back to mostly normal. After a few weeks of work, I was making it through a full day without the need for a break, although I was still making an effort to take them.
Being busy helps too. Work got busy and kept me distracted. And then we bought a house, and I went from busy to overdrive. Moving is both mentally and physically exhausting, but I actually improved through it! The week we moved I found that I no longer needed Tylenol daily. I did worry that I was doing a little more than I should (we had movers come, but I did a lot of the packing and unpacking) but Dr. Skaggs said it was all OK to do, and in the end, I think it made me stronger. In fact, it made me appreciate the benefits of the surgery even more because that type of physical strain would have actually taken an even bigger toll in the past. I still have minor aches daily, mostly stiffness from being in one position too long, some soreness where the hardware is close to my skin, and occasional muscle spasms. But there are times when I don’t feel it at all, all my old aches and tightness are gone, I don’t tire as easily, and maybe its just a coincidence but I’ve had much less frequent headaches.
At my 3 month appointment, Dr. Skaggs declared me “perfect” and a “poster adult” for the surgery. I don’t need to return until my 1 year anniversary. His biggest piece of advice was to get back to all exercise, and “don’t hold back”. This was mainly in response to my complaint that my shoulder was still a little achy. I was considering therapeutic massage, which he said was fine to do, but that I might get a better result with exercise. And he was right. I’ve started back with regular mat Pilates classes and some swimming and it is already helping, although I need to be doing it more often. I’ve gained all my weight back, and its time to start acting like a healthy 30-something who just needs to stay in shape. So that’s my new goal. Normal exercise.
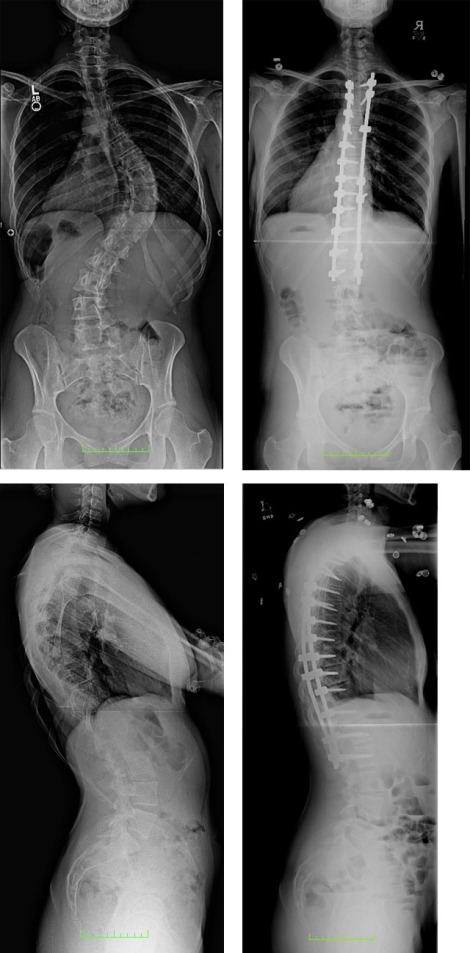
Below are my before and after x-rays, plus some photos I took about a month ago compared to “before” photos from last year. You can see my lumbar is still compensating a bit, and my left shoulder is hiked up, but overall a huge improvement!
- 5 comments
- Posted under Uncategorized
June 23, 2012 3 Weeks Post Op
It’s been three weeks since my surgery and I’m now much less sedated and have the energy to recap some of the details of it all. But a lot has happened, and some of the memories are now hazy, so I’ll do my best to sum it up. To start with the surgery itself went very smoothly, even better than Dr. Skaggs expected. It took just over 4 hours and did not require a blood transfusion. They fused one less level than expected — from T3 to L2 (originally planned to include T2 as well). And Dr. Skaggs got an excellent correction, better than he expected for a non-adolescent.
I was in the hospital for 4 nights and 5 days. Aside from a few isolated incidents the nursing staff was excellent. My husband stayed with me in my room the entire time and did an amazing job of comforting me and being my advocate when I needed help. When I first woke up in the recovery room the pain was pretty awful, but they soon got it under control. I was on a dilaudid IV drip with a pump I could press every 8 minutes if I needed it. I clutched that button for the first few days like there was nothing else in the world.
Every day in the hospital some little bit of progress was made. The morning of Day 2 (1 day post-op) I sat up at the edge of the bed and took two steps to sit in a chair briefly. That was terrifying. I was shaking, couldn’t catch my breath, and had tears in my eyes. I was sure I couldn’t do it, but I did. And that night I took my first shuffle around the room. The next day I left my room for my first real walk around the hospital floor. After that they deemed me mobile enough to remove the catheter which I could not get rid of soon enough. And soon I was a pro at log rolling and getting in and out of bed by myself. The next day I took a longer walk — a full loop past the nurses station instead of just down the hall and back.
The hard part was switching from the IV drip to taking pain meds orally. They stopped the automatic drip first, but I still had my pump for emergencies. The trouble was I would fall asleep and wake up in horrible pain because I hadn’t been hitting the button. But my husband and the night nurses did an amazing job of calming me at those times and finding solutions. Ice chips and the green light on the pump were my best friends. Even up until the day I was discharged they were still giving me injections for breakthrough pain. But the pain management team came up with a solution of combining both oxycodone and oxycontin to give me the coverage I needed when I got home.
The only trouble was getting the prescriptions filled was surprisingly difficult. Due to a mix up we didn’t get the prescriptions until late in the day. My husband went to the hospital pharmacy to fill them so we would be sure to have what we needed when we got home. But they were all out of oxycontin. He started to call around to nearby pharmacies but as soon as he said “oxy-” he would get an abrupt no. We couldn’t risk the hour plus drive in rush hour traffic to get to our own pharmacy. I needed a pill every 2 hours at that point. Luckily a nurse came through, calling a pharmacy for us, unfortunately it was 20 minutes in the wrong direction. So I stayed behind at the hospital while my husband went to fill it. It was 8 pm by the time we were ready to start the journey home.
It was a relief to be back in the comfort of our own home, but it was also scary. We were on our own now. It helped knowing that we had the personal cell phones of my surgeon and his staff, and they even called to check in at first. But we were still in unknown territory. My husband ran himself ragged for two days trying to arrange things around the house for me (we did some of this beforehand, but there were still things we hadn’t accounted for). And for some reason that first morning I woke up nauseous. I took two bites of my breakfast before throwing up in the kitchen sink (a scary prospect considering I couldn’t really bend forward so I was actually glad I wasn’t closer to a toilet). Luckily this has been my only real run-in with nausea the entire time. Constipation on the other hand was a bigger problem. I didn’t “go” for 7 days despite being on a regiment of stool softeners. The thing that finally did it was when I held my nose and drank a cup of warm prune juice.
A couple days after we got home, my mom and step dad arrived. At that point I was pretty much mobile and able to care for myself, but they helped with meals and cleaning to give my husband a break, but really just by being there they were a big help to me. It gave me a little extra motivation to get out of bed and hang out wherever they were. We spent a lot of time just sitting in the backyard in the sun and they accompanied me on walks. I started out walking short distances outside several times a day. We live in a very hilly neighborhood so it was hard to go far at first, but every day I would walk a little farther. I now walk a mile in the morning and a mile in the afternoon every day. I cried when my parents left. Granted, this whole time has been filled with tears, some warranted and some for no reason at all. But now I was really on my own (my husband had to return to working, though still in house). So I had to be my own reason to get out of bed. And at the same time, I was no longer making exciting progress every day. Things had leveled off, and there were less and less milestones to celebrate.
On Monday I had my two week follow up appointment. They were very happy with my progress and I’ve been cleared to do any and all activities I please, except for drive because I’m still on narcotics. Dr. Skaggs didn’t see any reason to measure my post op curve, but when I pushed him he quickly measured it and said it was probably about 11 degrees — better than I could have ever imagined! I am still leaning to the left a bit, but he feels this is a result of my lumbar having to compensate all these years and that it will work itself out in a few months. They gave me my prescriptions and a couple rolls of tape to cover the scar and keep it from stretching and sent me on my way. I’m not due for another appointment for three months, but I know how to reach them if anything comes up.
Now I’m working on weaning myself off the pain meds. I’m completely off the oxycontin, and working on reducing my oxycodone. It’s nice to come out of the fog a bit, but at the same time it’s frustrating. I’m still in a good amount of pain, discovering new pains as things begin to “wake up”, and I’m also experiencing what I think are some symptoms of withdrawal. On top of that, now that the swelling has gone down, I’m more aware of the restrictions in my range of motion. I’m no longer making exciting progress so I have to keep reminding myself that I won’t feel this way forever. I just wish I knew what my new normal will feel like so I know what I have to look forward to. At this point I am glad that I went through with it, but only time will tell what the future holds.
But on a positive note I’m now 1 1/2 inches taller, have a waist, and I’ve lost about 5 pounds despite the added hardware! I’ve requested copies of my x-rays from the hospital so I will post again when I receive them, and maybe post a few photos too.
- 9 comments
- Posted under Uncategorized
April 27, 2012 Surgery June 1st
It’s official. Surgery is scheduled for June 1st with Dr. Skaggs and Dr. Goldstein assisting. Finding a date that fit in with everyone’s lives – both doctors, hubby, mom, work – wasn’t easy, and everyone had to compromise a little, but I’ve learned there’s no perfect time. I also found that it wasn’t enough for just me to be emotionally ready, I needed to be patient for everyone around me to get there too.
Now that its official, I’ve moved into preparation mode. I’ve notified work and started the ball rolling on short term disability. I’m making sure all my ducks are in a row with insurance. My mom is taking off work starting June 8th so she can be with me the week I get home. The spring cleaning bug / nesting instinct is kicking in – cleaning out the old and collecting new supplies for my hospital stay and when I get home. And I’m attempting to whip myself into shape, especially my cardio health. All of these are nice distractions as the nerves also kick in. I’ve found exercise to be the perfect counterbalance so that I can sleep at night.
I don’t think I’ll be posting as much these days. My journey has been somewhat unique up until now. Looking back, its actually the journey of how I’ve come to terms with surgery. But there are many surgery stories out there with plenty of info about grabbers, pain meds, and stool softeners. Everyone likes to hear that someone made it through OK, but the real test comes 10, 20, 30 years later. I’ll periodically check in and update my story, but I’ll leave the blow by blow accounts to someone else. Don’t get me wrong, they’ve been extremely helpful for me to feel comfortable with the whole process. But there’s no shortage of it out there, so I’m going to let myself be “in the moment” for this with no feelings of obligation to the internet.
I have my pre-op visit mid May. They will be doing a full physical exam, taking new x-rays, and also completing paperwork. My husband will be coming to this visit so he can meet Dr. Skaggs, and I’m starting to prep a list of questions to remember to ask. Wish me luck!
- 10 comments
- Posted under Uncategorized
January 29, 2012 Wisdom Now Extracted
Three weeks ago I finally had my wisdom teeth removed. Just like scoliosis surgery, its something doctors have been telling me to do for years, but I ignored them because I was doing just fine as is. Unlike scoliosis surgery, it was easy. I had a nice quick nap, truly enjoyed my time coming out of the anesthesia, and then was pain free for about 12 hours. For a week I had a dull ache in my jaw that was controllable with ibuprofen, but that was my biggest complaint, aside from having limited food choices.
While I know this really won’t compare to the big one, in some ways it was practice for my husband and I. For one, I feel much more comfortable with the idea of anesthesia. At the very least I know I don’t react poorly to it, although the memory issues were very frustrating. But my husband was right there with me to get me home safely and remember all the instructions we were given.
But the eye opening part (pun intended) was the inadvertent benefits of whatever they gave me through the IV. I walked in with low back pain, and a slight headache/eye strain because I had to wear my glasses. But I walked out without any pain at all. This raises all kinds of chicken vs. egg questions about my eye issues. Is it all caused by neck strain? Or was I just too loopy to notice any issues, and therefore not straining? I wish I had thought to ask what they gave me. Not that I’m interested in taking narcotics, but its nice to know there’s something that could help me if I needed it. Sometimes it takes being pain free for me to realize that’s an option.
- 8 comments
- Posted under Uncategorized
January 29, 2012 Aches and Pains
I’ve been so focused on the big decision that I haven’t been doing a good job of tracking how I’m feeling physically. The truth is that I haven’t been keeping up with the Schroth exercises, and I’ve pretty much weaned off the brace. It started when we took a long weekend trip and I chose to leave the brace behind. By the time I got home I was desperate to put it on and feel that nice stretch. After that I started having pain in my low back and rib hump, mostly just when I would get up from sitting, or bend down to pick something up, and occasional spasms in my rib hump.
At that point I was still using the inversion table and sleeping in the brace most nights. I felt dependent on the brace for a good night’s sleep and to wake up without any aches and pains. But my eyes were causing me a lot of trouble — blurry vision, very bloodshot, and pretty frequent headaches. The good news is I haven’t had a single full blown visual disturbance episode since quitting the pill and starting the diet. It’s clear that the diet makes a difference because the week before Christmas I splurged on nuts, chocolate, and anything that arrived in a gift basket, and I paid the price with headaches.
But I was worried that the brace or the inversion table or both was somehow inadvertently causing strain or pressure in my eyes. The brace was also starting to feel very snug in the belly area. I don’t know if it was a result of the brace, getting older, lack of exercise or all of the above, but my stomach was the largest its ever been. So I decided to go cold turkey for a bit. It seems to be helping with my eyes/head, but its a trade off. Now the pain in my lower back seems to be worse, almost constant, although still low grade and very manageable, but it is also now shooting down my left leg, something that I used to get in my yoga days.
But now I have a new symptom. I call it a leg hotflash, where my left shin suddenly feels very hot, almost like someone turned on a space heater right next to me, but the skin is not red or hot to the touch. From a little Googling I found that it could actually be hormonal (I have been having trouble regulating since quitting the pill) or it is very often related to lower back pain/pinched nerves. When I got my MRI report it did say that I have a herniated disc at L2-3, but it seems like most of my pain is below that in the sacrum and legs. In fact, I started doing some hip stretches and it seems that that stopped the leg hot flash for about a week before it came back. I’ve also had some new strain in my left arm, shoulder, and wrist. I’m thinking of switching my mouse back to the right just to give it a break.
Everything I’m feeling is real, but there’s definitely also a psychological component. When I was focused on exercise, everything felt great, even the new pains are just my body adjusting. When I’m thinking I need surgery, my body gives me a reason to believe that I’m falling apart and will only get worse without it.
- Leave a comment
- Posted under Uncategorized
December 28, 2011 Timing Is Everything
I’m the type of person that once I’ve made my mind up, all I want to do is push forward. I am not a dawdler. But am I jumping into the deep end before I can think about the temperature of the water? NO. I’ve known about my scoliosis, and been a surgical candidate, for 18 years. I’ve spent 17 of those years hearing only the negatives of surgery, and believing that I can avoid it. I’ve spent the last year learning as much about the realities as I can, not just the worst case scenario fears. And I’ve spent the last 4 months getting as many opinions on my particular case as possible.
But before I get too caught up in it all, I want to methodically think through all the reasons why I now feel its the right time. David Wolpert’s book, “Scoliosis Surgery: The Definitive Patient’s Reference“, which I read maybe a month ago, does a good job of summing up the indications for surgery along with factors to consider when deciding when is the right time. Below are the indications listed. Any one of these is enough to qualify as a surgical candidate by surgeons standards (the book doesn’t spend much time exploring other options, but that doesn’t mean there aren’t other solutions worth exploring for some people even if they qualify for surgery.)
“Your curve currently exceeds 50*”… Yes, no doubt about it. Although the same x-ray has been measured anywhere from 57-70* depending on the doctor.
“Your curve is progressing”… I don’t have enough documentation to show whether it is progressing rapidly or not. But we know that curves over 50* tend to continue to progress in adulthood by about 1* per year. Based on my measurement at first diagnosis and my latest measurement, it seems that I likely am progressing at the usual rate.
“You have severe or chronic back pain attributed to scoliosis”… I would say no to this. I do have some back pain, and have good days and bad, but I wouldn’t call it severe and I don’t know whether it would fall within the realm of common back pain that all adults experience regardless of other back issues. I also have migraines that scoliosis may or may not be contributing to.
Wolpert also lists contraindications, that may be a reason NOT to have surgery even if the above is true…
“You are too old”… Not yet. In my opinion this would be a vote for doing it sooner than later.
“You are in frail health”… Nope. Again, this makes me think I should do it while I can. You never know what the future holds.
“You are an addicted smoker and unwilling to quite”… Nope.
“Your primary objective is to improve your cosmetic appearance”… This definitely wasn’t one of my main reasons to start seriously considering surgery. But if I’m being honest, I’d have to admit that as surgery becomes more of a reality, I can’t help but be excited about the idea of being straighter. Since I don’t have any major changes in pain or function to look forward to in the short term, this gives me an immediate benefit to look forward to rather than just the long term benefits which are much harder to appreciate.
“You have no support system for recovery”… While it will require some changes in their schedules, between my husband and my mom I know I’ll be covered. My husband’s softer side truly comes out in his bedside manner. And my mom, who would come stay with us, is an occupational therapist. She does home visits, mainly to the elderly, after they have come home from a hospital or rehab stay to make sure they can function safely. She’s already well versed in no BLT (bending, lifting, or twisting), and is excellent at sourcing a raised toilet seat, but really I’m pretty sure I’ll just need my mommy.
Clearly I pass the test. I already knew this because every orthopedic surgeon I’ve ever seen has told me. But it helps to organize my thoughts into these logical categories. Without them, the mind starts to wander into all the little details and irrational fears, and its easy to lose perspective.
But then there are the “when” factors…
“Availability of caregivers”… My husband is in the midst of a life-changing career move that will make things difficult because it requires a lot of his mental focus right now. Logistically he is working from home for now so he would never be too far away if I really need help, but its hard to predict his schedule past the next 6 months, he could be away from home quite a bit after that. My mom can fly out any time, although she’s anxious to know a timeline so that she can plan around it and request the time off.
“Work”…My direct supervisor knows that I’m considering surgery and is very supportive. I’m not worried about the stability of my job, as long as I’m respectful of scheduling. From that standpoint, we currently have a freelancer filling in for my counterpart who is on maternity leave. She is due to come back in March (assuming she can leave her baby’s side) so it would be easy to slip away at that time and keep the freelancer on a little longer.
“Your health insurance”… It’s not the best but at least I have it. My husband’s is also changing and may be a lot better than mine, but I’m reluctant to switch over in the midst of this and trigger any preexisting condition red flags.
“The weather”… It’s LA so not a major factor but the first few months of the year tend to be pretty rainy which would make walking less appealing.
“Getting your life in order”… Not too worried about this, I’m pretty good at organization.
“Pregnancy”… This is my big reason to do it in the next year. Even if all goes well, I’ll need at least a year to recover before we can even think about kids. Tick tick tick.
For me, all of these factors add up to March of next year. It feels really soon, but I would hate to put it off out of fear only to have some other obstruction come up in the future. I’ve reached out to Dr. Skaggs to coordinate his and Dr. Goldstein’s schedules, and I imagine I’ll here back soon after the new year. I’m sure there will be many moments of panic in the days ahead, but I have for the most part learned to make my peace with it. I no longer cry at the thought of surgery, and am actually starting to find little pleasures to look forward to.
- 4 comments
- Posted under Uncategorized
December 28, 2011 One Final Opinion
Last week I spoke on the phone with Dr. Weinstein in Iowa, the last opinion I will be seeking. While we haven’t met in person, he reviewed all my studies and asked me all the usual questions about my history with scoliosis. He came to the same conclusion as all the other surgeons — that I have all the indications for surgery. He made a point to say that that doesn’t mean that I have to to do anything. Its possible that I won’t ever need surgery, and some people do choose to hold out as long as they possibly can. But on the other hand, he agreed that for the least risk and best outcome, sooner is better than later.
He saw it as a straightforward posterior selective thoracic fusion, and opposed the notion of a minimally invasive approach. I asked if he felt it was worth traveling to him or any other top guys in the country, and while he said we would be happy to treat me, he actually recommended against it. People travel for surgery for a variety of reasons, he said, including to LA. But he didn’t see any benefit that outweighs the comfort and support system of home, and the reassurance that your surgeon is nearby if needed.
He left me with the names of what he would consider to be the top scoliosis surgeons in California (by reputation, not by personal experience):
- David Skaggs, LA
- Serena Hu, San Francisco
- Peter Newton, San Diego
- Behrooz Akbarnia, San Diego
I told him my reservations about Dr. Skaggs’ practice being focused on kids and teens, and he didn’t see that as a concern. The surgery is the same, he said, and any good doctor is conscious of their individual patient’s needs. And since I’ve already met with Dr. Skaggs and liked him, and he is the closest to me, I’ve come to the conclusion that WE HAVE A WINNER! I’ve contacted his office to get the ball rolling. Holy expletive, I think I’m doing this.
- 8 comments
- Posted under Uncategorized
December 1, 2011 Metal Allergy
This week I went to see an allergist to get tested for the most common metal allergies. I’ve had skin reactions to earrings in the past so if I’m going to have a back full of rods and screws I want to be sure I’m not going to have a reaction that leaves me miserable and requires a second surgery for hardware removal. And it turns out I was right! I am severely allergic to nickel which is a common allergy among the metals and often surfaces from a reaction to cheap jewelry. This type of reaction is called contact dermatitis. It doesn’t guarantee you will have a reaction to implants too, but better safe than sorry!
In talking to different surgeons different types of instrumentation have been mentioned, including cobalt chromium, stainless steel, and titanium. All are alloys that contain other trace elements. According to Wikipedia, cobalt chromium and stainless steel usually contain some nickel, but titanium may not…
Titanium
Stainless Steel
Cobalt Chromium
I will of course confirm exactly what is in any instrumentation with my surgeon. And I don’t plan to base my surgeon decision on the type of instrumentation they usually use, but instead choose my surgeon, and then be sure they understand my allergy and are comfortable adjusting to a different type of instrumentation if necessary. Now that I know I have at least one metal allergy, I’m thinking I may even get tested for any additional metals in whatever instrumentation is recommended
On a side note, the allergist also tested me for all the common airborne allergies like pollen, dust, mold, and pets, and all were negative! This is what I was expecting but it helps confirm for me that all my head issues are migraine related, not allergy related. Although he made a point to say it doesn’t mean that I wouldn’t still react to pollution or other direct irritants in the air, and things did get worse about a year after moving to LA. One mystery solved, but many more remain…
- 13 comments
- Posted under Uncategorized
November 21, 2011 Too many opinions
I’m falling behind on my posts. But more importantly, I’m exhausted, frustrated, and spun in circles. Last week I got a call from Dr. Goldstein after he had reviewed my films and consulted with Dr. Skaggs. Apparently Dr. Skaggs, although usually only sees children, wanted to see me. He told me that both Anand and Pashman are good doctors, but if I want the best, go to Dr. Skaggs. The same day I got an email from my dad’s friend telling me that Dr. Weinstein in Iowa would be happy to see me.
I went ahead with a follow up I had scheduled with Dr. Pashman for Friday. Like Dr. Anand, I felt that he was too busy defending his method and debating MISS to give me a straight answer about anything. I’m starting to see some of the personality quirks others have mentioned. He first told me that my curve bent out to 45*, and when I questioned it (because Dr. Anand measured it at 24*), he went and measured and came back saying my curve is 70* and bends out to 32*. I can’t help but think that he is estimating high in order to fit his argument that I have a “stiff adult curve that needs to be worked at”. He would fuse from T2 or T3 to L1. He also seemed to drop the spina bifida discussion with no explanation. I can tell that he is good at what he does, and does a lot of it. I’m just not sure why he’s in it.
Then today I visited Dr. Skaggs. He is both warm and respectful just as I expected. And I also felt out of place being handed pediatric forms, just as I expected. What I didn’t expect is that while he very rarely operates on adults, he wants to operate on me with Dr. Goldstein assisting. He suggested that this way I would have both his expertise with correcting scoliosis, and Dr. Goldstein’s expertise with adult pain management. I was both amazed that they were willing to do this for me, but also felt lost in the political drama playing out between the surgeons. I had no idea just how competitive they are. He told me flat out that if I were his daughter he wouldn’t go with MISS, and isn’t sure that it has as good a fusion rate as the traditional procedure. But he was very thoughtful with all my questions, took his time and answered them directly, and was very clear that there is a lot of gray area. He reassured me that in my case there is no wrong decision. The only concern I had with him is that he wanted to fuse from T4 to L3. When I expressed concern with going that low, he re-evaluated and said that it may be L2, but definitely not L1 as Pashman proposed. As long as he’s not just doing what I want, I respect his willingness to change his mind, especially since he said he prefers to sit alone for a while to make that decision.
At some point there might be such a thing as too many opinions. They all start to cancel each other out. The only thing they can all agree on is that I need surgery. I like the idea of the dream team, but I’m also worried about confusion with the staff if its not a routine case. Dr. Goldstein was supposed to by my decider, but now he’s worked his way in. So I’m hoping Dr. Weinstein will be the new decider. I ordered copies of my studies today and will be sending them off for his opinion.
- 1 comment
- Posted under Uncategorized